PCOS & fatigue: What is the link between PCOS, sleep and fatigue?
Living with PCOS can be challenging and overwhelming. Its diagnosis is complicated and so are the symptoms associated with it. PCOS not only affects women’s health on many fronts, but it can also interfere with one of the most basic human needs: sleep.
If you have PCOS and feel constantly tired, this is the right post for you! Here, we will examine the link between PCOS and fatigue and how this can impact on your sleep, and we will look at possible ways to manage fatigue and the sleep disturbances associated with PCOS.
PCOS: Definition and symptoms
Polycystic Ovary Syndrome (PCOS) is a common cause for female infertility affecting 1 in 10 women (1). This endocrine disorder is characterised by higher than usual androgen levels (male-like hormones), irregular menstrual cycles, polycystic morphology of the ovaries and insulin resistance (2).
There are a variety of symptoms associated with PCOS including acne, oily skin, rapid weight gain, irregular periods, difficulty getting pregnant, excess body hair, hair loss and fatigue (3).
Does PCOS cause fatigue?
Although PCOS is not a direct cause of fatigue, there is emerging evidence suggesting that sleep disturbances are a common feature in women who suffer from the disease (4) which can then have a knock on effect and cause fatigue and tiredness.
Sleep disturbances refers to a wide range of sleep disorders such as insomnia (difficulty falling asleep and maintaining sleep), hypersomnia (excessive daytime sleepiness ) and obstructive sleep apnoea (OSA) which is the most common sleep disorder among women with PCOS (5).
A 2014 study looking at sleep in 87 women with PCOS and 673 women without PCOS found that sleep disturbances were twice as common in those with PCOS than those without. Especially common in those with PCOS was an increased difficulty falling asleep and interestingly this link was independent of body size and depressive symptoms (6).
Additionally, lack of sleep is associated with weight gain, mood and memory changes, worsening of insulin resistance, increasing the risk for high blood pressure and type 2 diabetes and can even contribute to chronic inflammation (7)
Sleep Apnoea and PCOS
OSA is characterised by episodes of complete breathing cessation during sleep, and it is estimated to affect ~40% of women living with PCOS (8).
There are many potential factors linking PCOS and OAS, one of which is body size. Some research discusses a link between being in a bigger body and increased risk of OSA due to excess weight contributing to collapse of the upper airways which blocks the flow of air. However, recent research suggests that the increased risk is more likely due to having high amounts of a specific type of fat tissue called visceral fat, rather than excess overall weight (9).
Visceral fat is fat tissue which is wrapped around organs like the liver, stomach, lungs etc. affecting how they function. It has been found to be more metabolically active, meaning it interferes with some of the body's normal processes (such as metabolising or processing sugar or glucose) more than other types of fat tissue, and this is why it can increase risk of insulin resistance developing. Having OSA can therefore contribute to worsening PCOS symptoms. In addition to this, by causing fragmented sleep, OSA increases cortisol levels (the stress hormone) which then lead to oxidative stress (that can cause cell damage) and insulin resistance. What a vicious cycle!
Fatigue and PCOS
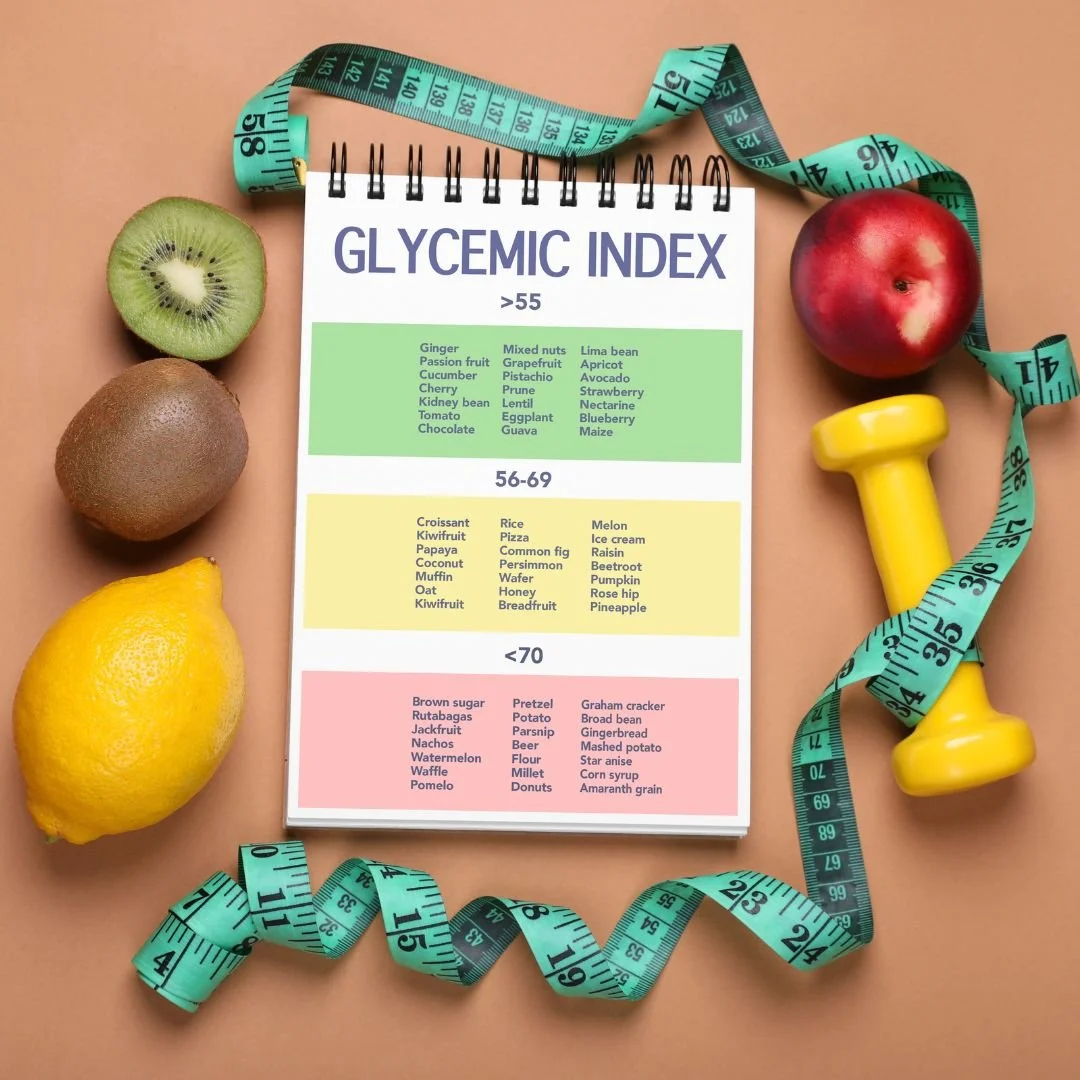
Fatigue in PCOS may also be attributed to insulin resistance (IR) and the fluctuations in blood sugar levels that come with it (10). It is estimated that 75% of women with PCOS are insulin resistant, meaning that although their pancreas makes and releases insulin (the hormone that allows our bodies to use glucose), their cells are unable to use it correctly (11). This causes abnormal blood glucose spikes after meals, especially those high in carbs. This chain mechanism ultimately affects energy levels, leading to fatigue in women with PCOS (13). Choosing carbs which have a lower glycemic index (a value that indicates how each food affects blood glucose: the higher the GI, the quicker the blood glucose levels will rise and the higher the glucose spike will be) (12) can help to manage insulin resistance in PCOS.
As if this wasn’t enough, anxiety and depression, which are 3 to 4 times more common in people suffering from PCOS, are also associated with sleep disorders (14). With all these factors having an impact on sleep and energy levels for those with PCOS, know that you are not alone if you have been struggling for a while to fight your fatigue.
But don’t worry, next we’ll find out what you can do to improve your sleep and your overall energy levels. Keep reading!
Tips for Managing Sleep and Fatigue in PCOS
Optimising Sleep
Now that we’ve revealed some of the ways PCOS and fatigue are correlated, it’s time to look at the actions you can take to reduce fatigue by prioritising and improving your sleep quality (15).
Avoid caffeine for at least 6 hours before bedtime- caffeine consumption close to bedtime delays sleep onset
Avoid smoking: nicotine decreases total sleep time and causes early morning awakenings
Avoid alcohol before bedtime: alcohol is known for causing lighter sleep with frequent sleep interruptions
Exercise regularly: moderate intensity physical activity has been found to decrease the intensity of OSA (16)
Get into a sleep routine: regular sleep-wake patterns are associated with better sleep quality so aim to go to bed and wake up at the same time every day, even on weekends if you can
Avoid technology use before going to bed: the blue light of LED screens causes a delay in melatonin surge (a hormone that promotes sleep) (17)
Reducing Fatigue
Remember insulin resistance and those blood glucose spikes that cause you to feel exhausted throughout the day? For those there is a quite simple tip:
Try to choose low GI foods over high GI foods as often as possible. For some examples of low GI foods check out this IG post!
PCOS has a variety of symptoms including sleeping disorders and fatigue so learning how to manage fatigue and getting a good night sleep can be an important part of your PCOS treatment. Making small adjustments to your diet and implementing simple lifestyle habits discussed in this blog can help you feel revitalised, minimise any daytime slumps in energy and get good quality uninterrupted sleep, all of which can improve your quality of life.
If you are looking for more personalised support, book in a discovery call work 1:1 with Dr Claire Pettitt by following the link https://www.clairepettitt.com/contact
References
Sleep disturbances in a community-based sample of women with polycystic ovary syndrome
Metabolic dysfunction in PCOS: Relationship to obstructive sleep apnea, Steroids
Fundamental Concepts and novel Aspects of Polycystic Ovarian Syndrome: Expert Consensus Resolution
Real-Time Associations Between Glucose Levels and Fatigue in Type 2 Diabetes: Sex and Time Effects
Anxiety and Depression in Women with Polycystic Ovary Syndrome
Systematic Review of Light Exposure Impact on Human Circadian Rhythm