Dietary Strategies for Managing IBS
Irritable Bowel Syndrome (IBS) is one of the most common functional gastrointestinal disorders globally (1). In Irritable Bowel Syndrome (IBS): The Basics, we explored what IBS is, what causes IBS, the signs and symptoms, who can develop it and general lifestyle management advice. This article will focus on some of the common dietary strategies out there that can help in managing the symptoms of IBS.
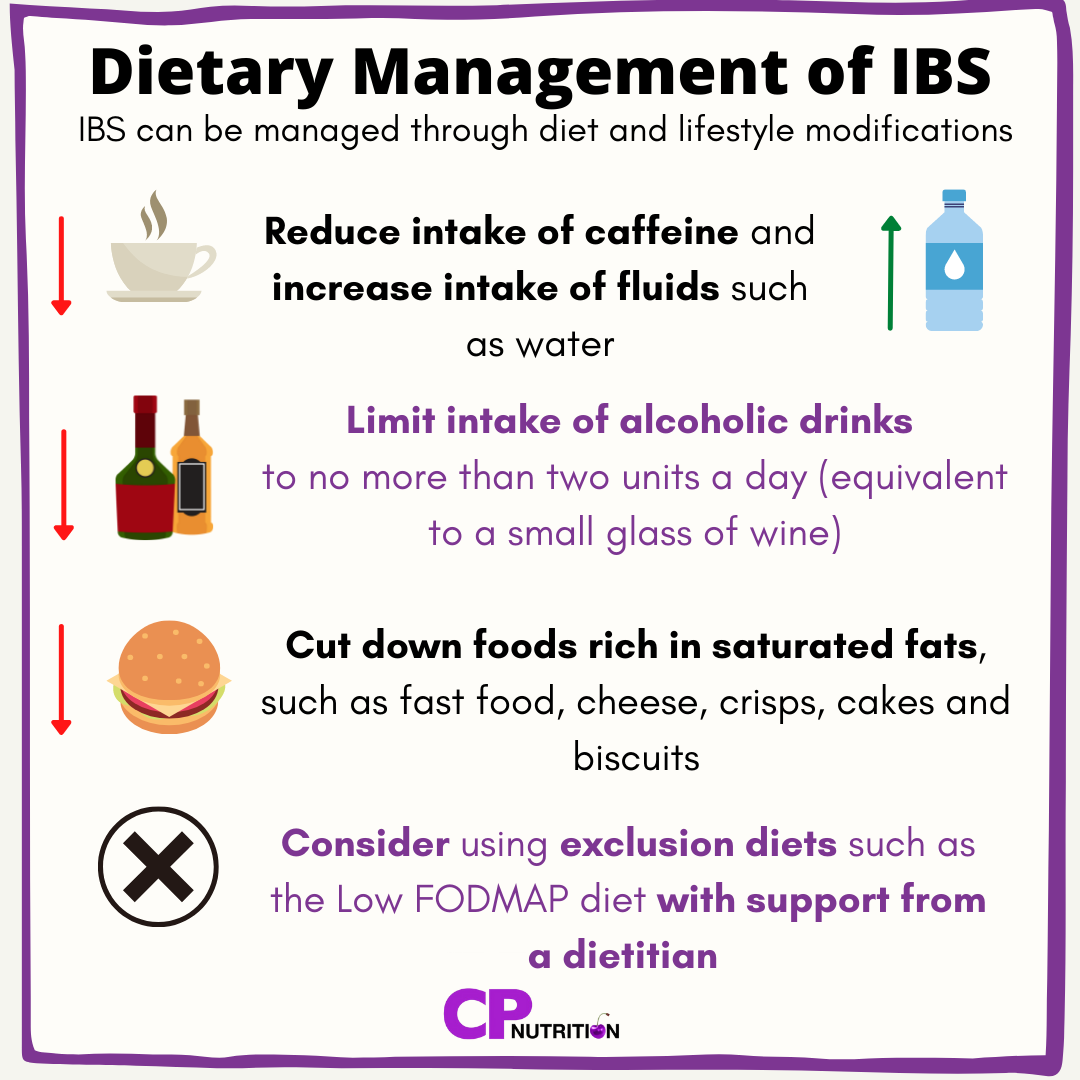
Dietary management of IBS
As IBS is a syndrome (or a collection of symptoms), each person with IBS can have a difference collection of symptoms (from diarrhoea, to constipation, to pain, bloating or gas) and so management of IBS with diet needs to be tailored to the symptoms the individual is facing. There are some general dietary strategies which may improve IBS symptoms which we tend to refer to as ‘first-line advice’ which are a good place to start when trying to manage your IBS, and these are listed below (2):
Reduce intake of caffeine containing drinks such as coffee and tea, to no more than three cups per day
Reduce intake of sugary/fizzy drinks
Alcohol intake should be limited to no more than two units per day
Try to consume around 8 cups of fluid per day (such as water)
Reduce consumption of foods rich in saturated fats, such as fast food, pizza, cheese, crisps, cakes and biscuits.
Dietary Fibre - friend or foe?
Fibres are carbohydrates that can’t be digested, and there are two types: soluble and insoluble.
Soluble fibre is easily dissolved and can be found in vegetables, fruits and oats.
Insoluble fibre does not dissolve and is common in legumes, seeds and root vegetables.
In those who are constipated, incorporating insoluble fibres to bulk out your faeces may reduce constipation, as this fibre will increase the water content of faeces and speed up the passage of food through the gut (3).
However, diarrhoea, bloating and gas in IBS may be related to the excessive consumption of insoluble fibre, and so if an individual suffers from diarrhoea-related symptoms, it could be beneficial to reduce intake of this and monitor for changes to symptoms (4).
So as you can see, IBS can be complex, and dietary changes really need to be tailored to your individual symptoms and circumstances.
Low FODMAP diet
Over the years there have been many dietary strategies considered for those with IBS, including encouraging diets high in bran (this is no longer recommended) (5) and following exclusion diets to identify trigger foods. For some people with IBS, certain foods may exacerbate their symptoms and therefore they may need to be either cut out or reduced. A food and symptom diary can be a useful way of monitoring for potential trigger foods (5).
For some people with IBS following a specific exclusion diet, such as the low FODMAP diet, with the support of a dietitian, may help identify potential trigger foods. Although this diet has been associated with an improvement in gastrointestinal symptoms for many people with IBS, it is important to note that it has also been associated with increased risk of some nutrient deficiencies, it tends to be much lower in fibre and results in unfavourable changes to the gut microbiome (6). If this is something you are considering trying then get in touch with a dietitian who can support you in ensuring you don’t over restrict your diet and end up with deficiencies.
Probiotics
Another dietary strategy in managing IBS is to include probiotics in your diet. Probiotics are often known as ‘good’ bacteria that can have beneficial effects on the health of an individual. They can do this by competing with ‘bad’ bacteria for space to live in the gut and essentially stopping the ‘bad’ bacteria from overgrowing and causing harm (7).
Role of probiotics in IBS
The gut microbiome is described as an ‘ecosystem’ which comprises all of the bacteria and microorganisms that live inside of your intestinal tract, which can influence your health and disease status (8). One of the possible triggers for IBS is thought to be infection-related, which may cause alterations in the gut microbiome of a person with IBS which can lead to the overgrowth of ‘bad’ bacteria, and can cause symptoms such as bloating (7). In IBS, the use of probiotics may inhibit the overgrowth of the harmful bacteria, reduce inflammation in the gut and possibly reduce the hypersensitivity of the intestines. This can then reduce the symptoms experienced in IBS, such as abdominal pain, diarrhoea and bloating (7).
Which probiotics can help?
Probiotics come in many forms - they can be taken as over the counter supplements which are either capsules or powders, or they can even be found in everyday food items such as yoghurt and fermented milk (8). Some strains of bacteria that are thought to have beneficial effects on IBS symptoms include (7):
Lactobacillus acidophilus
Streptococcus thermophilus
Bifidobacterium breve and Bifidobacterium longum (used in combination)
The Bottom Line
Diet can play a huge role in managing your symptoms of IBS. Changes can be small, such as reducing caffeine and alcohol intake, or larger, such as trying out the Low FODMAP diet. Not sure where to start? Reach out to your dietitian who will provide tailored advice on what changes to make to improve your symptoms, and how to make those changes.
References
Chatila, R., Merhi, M., Hariri, E. et al. Irritable bowel syndrome: prevalence, risk factors in an adult Lebanese population. BMC Gastroenterol 17, 137
BDA, 2022. Irritable Bowel Syndrome Food Fact Sheet. [online] Bda.uk.com. Available at: <https://www.bda.uk.com/resource/irritable-bowel-syndrome-diet.html> [Accessed 20 January 2022]
Algera, Colomier and Simrén, 2019. The Dietary Management of Patients with Irritable Bowel Syndrome: A Narrative Review of the Existing and Emerging Evidence. Nutrients, 11(9), p.2162
IFFGD, 2022. Diet and IBS - About IBS. [online] About IBS. Available at: <https://aboutibs.org/what-is-ibs/diet-and-ibs/> [Accessed 20 January 2022].
McKenzie, Y., Bowyer, R., Leach, H., Gulia, P., Horobin, J., O'Sullivan, N., Pettitt, C., Reeves, L., Seamark, L., Williams, M., Thompson, J. and Lomer, M., 2016. British Dietetic Association systematic review and evidence-based practice guidelines for the dietary management of irritable bowel syndrome in adults (2016 update). Journal of Human Nutrition and Dietetics, 29(5), pp.549-575.
Van Lanen, A., de Bree, A. and Greyling, A., 2021. Efficacy of a low-FODMAP diet in adult irritable bowel syndrome: a systematic review and meta-analysis. European Journal of Nutrition,.
Dale, H., Rasmussen, S., Asiller, Ö. and Lied, G., 2019. Probiotics in Irritable Bowel Syndrome: An Up-to-Date Systematic Review. Nutrients, 11(9), p.2048.
Hong, S., 2014. Unraveling the ties between irritable bowel syndrome and intestinal microbiota. World Journal of Gastroenterology, 20(10), p.2470.